Sounding the Alarm
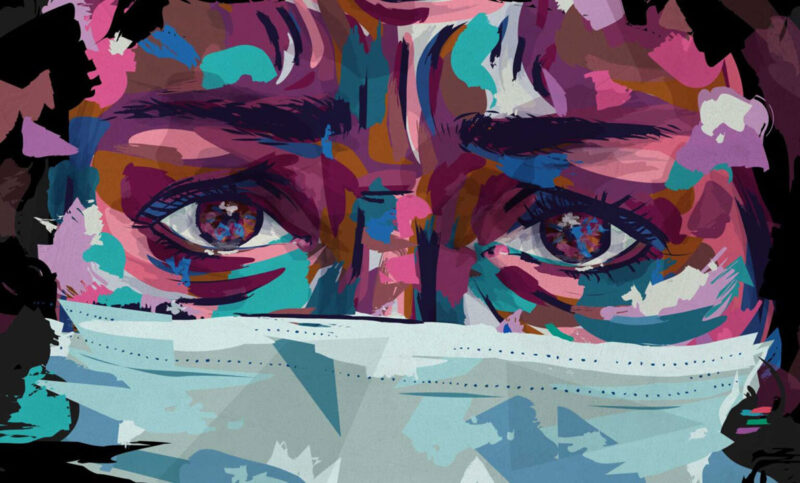
Jackie O’Halloran interviews Nurse Nacole, and the two sound the alarm on burnout, biases, and other issues pushing nurses to the brink.
“I haven’t properly been able to reconcile my feelings because it’s not good and bad, good and bad, good and bad. It’s been all like bad, devastating, bad, devastating, bad…I mean, even when I talk to just nurses, they’re like, ‘I’m over it.’“ —Nurse Nacole
Even before the pandemic, nursing was never an easy gig. We have always faced big challenges and intense pressures. From our patients to our colleagues, and even in our personal relationships, the dynamics of nursing are immensely difficult to navigate. All you have to do is look at the number of nurses who drop out of the profession within their first few years to understand the magnitude of the problem.
Now, with COVID-19, the situation is getting even worse. Nurses across the country are experiencing “COVID combat fatigue”—we’re exhausted, burned out, and genuinely wondering how long we can live our lives like this.
If you’ve been feeling alone in your frustration and your pain, we hope this special episode shows you that you’re not. We brought together two of our favorite SHIFT Talkers—our host, Nurse Nacole, and Jackie from “The Floor Is on Fire”—to tackle the big issues pushing nurses to the brink (and we let Jackie ask the questions this time around!). What we learned is that it doesn’t matter if you’re working in the Northeast or down South, if you’re white or if you’re Black, if you have an RN or an NP, or if you’re in your first COVID-19 surge or your fourth. All nurses are struggling. And while it’s certainly not a solution, talking about these tough issues is a start, an important one.
The toll of the ongoing pandemic
Jackie starts by asking Nacole about what’s on everyone’s mind these days—the pandemic. Working in Florida, where the pandemic has peaked multiple times, is understandably taking a toll on Nacole. She’s notified families that their loved ones have passed more times than she can count.
“I’m the one that has to call the families at night. So I have to wake them up, first of all. I’ve got to give them bad news…So it’s just draining to always be a part of someone’s worst experience of their entire life. And I’ve been doing that almost every shift for months now. So it’s just like, just being a part of that emotional process and always giving bad news. It weighs on you…my husband is like, ‘Hey, you want to go out?’ And I’m like, ‘No, I don’t want to leave my house. I’ve been involved in too many marriages that aren’t marriages anymore…’”
Nacole’s words show just how real pandemic exhaustion is. For some nurses, it’s been nearly nine months of treating really sick, isolated patients in overrun ICUs, in heavy duty gear, under the constant fear of getting the virus or spreading it to loved ones.
And even if your employer has stepped up (as we learn that Nacole’s has) and provided PPE and other critical support, at this point, many of us are as aggravated at the general public as we were or are at administrators.
“I trust my organization. They’re advocating for me. They’re doing what’s right. But statewide, it’s a bit of a dumpster fire, you know, with that whole thing. There are people protesting about wearing masks and then people spitting on each other and fighting, and it’s just like, ‘You know, guys, we’re all adults here.’ It’s getting a little out of hand. When I go to work, I feel safe. I feel unsafe when I leave work.”
How many of you feel safer at work than outside of work, SHIFT Talkers? You are not alone.
The role of race—not just during the pandemic but in the “before times”
It’s not just the pandemic that is chasing good nurses out of nursing. It’s also challenges that existed long before the crisis that will remain long after it fades–things like racial biases, gender discrimination, and disrespect in the workplace—substantive and significant challenges that make it impossible to say that nurses are quitting because of the stress of COVID-19 alone.
In the interview, Nacole shares her experiences with racism in healthcare from both sides of the hospital bed—as a Black patient and as a caregiver.
She discusses the vastly different experiences she and a white colleague had while giving birth just days apart at the same facility with the same OB-GYN, the fact that she rarely works with anyone who is her mirror in terms of race, and witnessing patients of color being treated differently and dismissed as “non-compliant” by default, especially when it comes to COVID-19.
“I said to another provider, ‘So you think that the pandemic is wrecking these communities and particularly African American communities because we are all non-compliant? Do you honestly believe that?’ Like, I know that there’s a level to that. There’s an aspect of that, but I just feel like [African Americans] aren’t getting the proper healthcare that they need.”
Nacole and Jackie also touch upon the role that their employers can play in addressing misperceptions about race and ignorant behavior stemming from them. Despite the differences in their backgrounds and professional experiences—Jackie is a white nurse and her hospital serves a primarily white community, while Nacole is a Black nurse working in a health system that serves a diverse community—both voice a strong belief that proactive conversations are key when it comes to combating racial injustice and that hospitals should facilitate true dialogue. A few slides on a PowerPoint training just aren’t enough. As we’ve heard many times and in many different contexts throughout this season of SHIFT Talk, education is the key to unseating ignorance.
“No one’s going to say, you know, ‘Hey, I’m a racist and hey, you know, I have all these biases from my past,’ but they definitely bleed into how they see experiences and how they manage certain patients.”
Which is why it’s so important for nurses to talk to each other and, as Jackie said, make themselves vulnerable by asking questions even when it’s uncomfortable.
And let’s not forget about gender bias—that’s a big one too
Nacole makes a really interesting point in the interview—that sometimes she can’t tell whether she’s being dismissed because of a racial dynamic or because she’s female. This leads to Nacole and Jackie spending several minutes talking about their common experience of being dismissed because of their gender.
“I feel like I don’t get taken as seriously. Like, if I say something and then a male says the exact same thing, what they say has more weight, even though we said the exact same thing, and I don’t understand where that comes from. And then just looking at them like, ‘Are you serious right now?’ Like, did [anyone] else see what just happened here?”
Consistently feeling unheard or disrespected in the way that Nacole describes makes nurses feel ineffective in their work, which is often yet another indicator of burnout (and that’s not even getting into the pay gap, which Nacole and Jackie do discuss on the podcast). Sensing a theme here, SHIFT Talkers?
Why we need to have more tough conversations
Conversations like the one Jackie and Nacole had are so important, and here’s why. For one, we all need to vent! And two, one day, the pandemic will not be the primary thing going on in our lives; we hope that day is coming sooner rather than later. And when that day comes, we need to have realistic expectations for ourselves—and for our administrators and executives—about what post-pandemic life needs to look like to keep more good nurses from leaving us.
Let’s keep talking and make the shift together.
