The Virtual Nurse Program in a Community Hospital Setting
By: Ruth Sagastume, MSN, RN, CPHQ & Jessica Peterson, PhD, RN
While nursing shortages are not new, the nursing profession is entering a “new era,” that challenges nurse leaders to create novel ways to provide adequate nursing resources and efficient patient care workflows. Virtual nursing care models are emerging as options to provide nursing services to support providers in the immediate bedside patient care environment. This article describes a virtual nursing care program implemented on medical-surgical acute care units to support inexperienced staff, maintain patient safety and quality, and improve patient care outcomes.
The nursing profession is experiencing a “new era,” challenging hospital leaders to effectively manage ongoing changes. As such, nurse leaders are responsible for teh creation of novel ways to provide adequate nursing resources and efficient patient care workflows. Constant pressure on operational leadership teams to develop creative models of care and, more importantly, to provide necessary support for an inexperienced nursing workforce, has been a significant factor affecting the stability of the nursing profession and healthcare systems in recent years (Brook et al., 2019; Edwards et al., 2015).
The call for nurses to use technology to redesign nursing care and promote patient safety is not new, and telehealth technologies have been available for some time (Cloyd & Thompson, 2020; Russell, 2023; Wakefield, 2008). Nurses have been instrumental in leading many telehealth initiatives (Lee et al., 2020; Yesenofski et al., 2015). Nurses’ use of technology increased substantially in the years prior to the COVID-19 pandemic, particularly in the areas of secure email and remote patient monitoring (Beauséjour & Hagens, 2022). The search for innovative care models that address nurse recruitment and retention within sustainable financial platforms continues to be a priority in healthcare. Additional virtual alternatives are emerging to provide options for nursing services to support the immediate patient care environment. One example is a hybrid virtual model, in which remote nursing care is provided in conjunction with in-person care (Russell, 2023; Schuelke et al., 2019).
Our community hospital, part of a large regional health system, began the journey with a hybrid Virtual Nurse Program approximately five years ago. At the time, the gap between nurse experience and the steady upward trend in patient acuity was affecting the work environment and daily operations within the telemetry and medical-surgical units. The relatively inexperienced staff, with many new graduate nurses, struggled to manage an escalating patient census, acuity, and the social and educational needs of the complex patients housed in these units. Stress on nursing teams was palpable at both facility and individual department levels; metrics related to employee engagement and bedside registered nurse (RN) turnover are reflective of this stress.
Virtual Nurse Program Principles and Goals
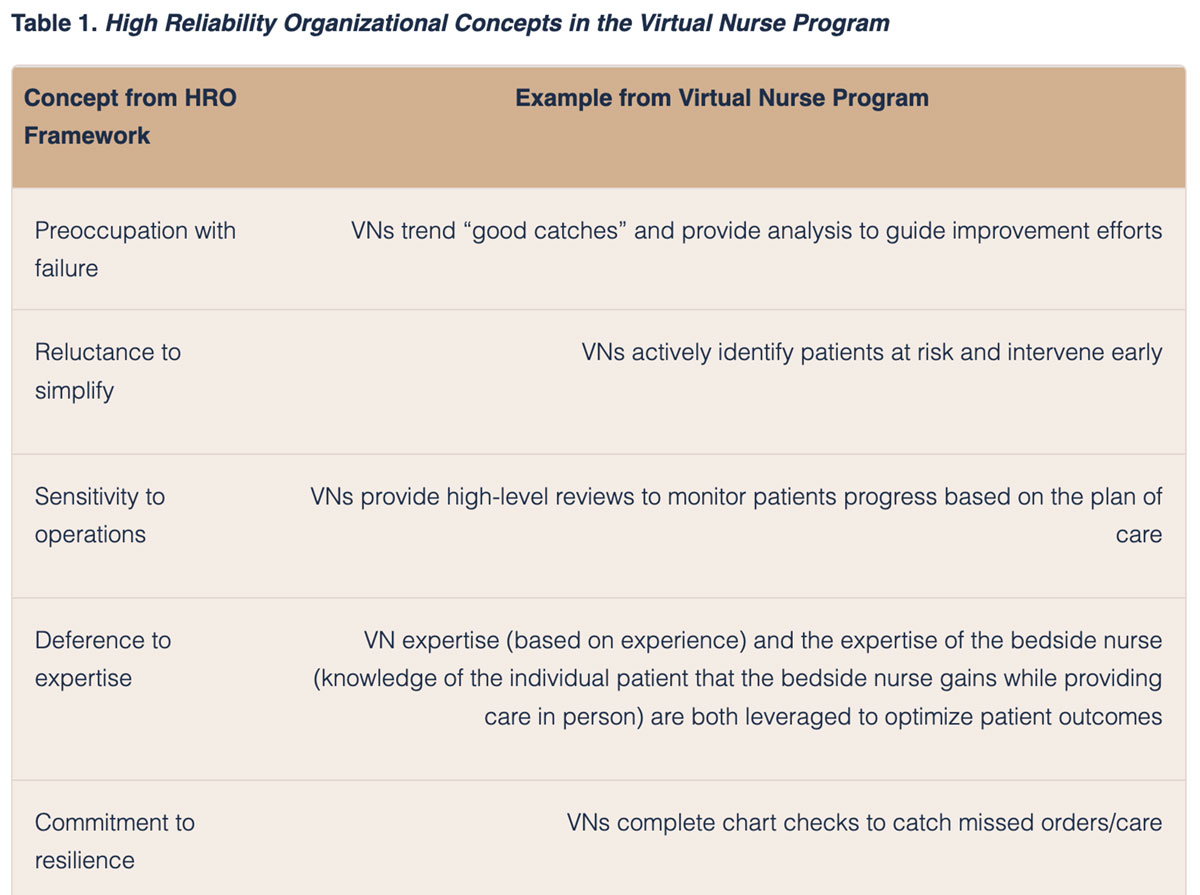
The implementation of the Virtual Nurse Program aligned with a high-reliability conceptual framework that the organization had embraced. The concept of high-reliability organizations (HRO) started within industries in which errors had significant consequences, such as aviation, and has been widely adopted within healthcare (Veazie et al., 2022). Five organizing principles or concepts guide HROs in improvement efforts to maximize safety (Hines et al., 2008; Veazie et al., 2022). These include:
- Preoccupation with failure, in that HROs recognize and intervene in the potential for failure, rather than waiting to react to errors.
- Reluctance to simplify, or the recognition that failures or potential failures may occur for any variety of reasons.
- Sensitivity to operations, in that HROs recognize that system activities may impact patient outcomes.
- Deference to expertise and empowerment of every staff member, regardless of position to identify patient care concerns and raise them for the team to address.
- Commitment to resilience, or the recognition that despite adequate systems in place, errors may yet occur.
In HROs these five principles guide the mindset of the organizational leaders who create systems in which safety is prioritized and high-quality care is consistently provided (Hines et al., 2008). Table 1 provides examples of HRO concepts within the Virtual Nurse Program.
The Virtual Nurse Program focused on supplying appropriate resources for the growing number of inexperienced nurses hired into telemetry and medical surgical areas, and on creating a care model that would optimize nursing labor through balancing tasks between remotely located virtual nurses and bedside nurses. The hybrid virtual model is designed to provide mentorship to novices and promote patient safety (Cloyd & Thompson, 2020; Russell, 2023). Goals of the initial pilot implementation of the program were to: 1) improve employee engagement and retention, 2) uphold financial standards, 3) maintain overall quality, and 4) avoid safety incidents. In this framework, the following objectives became the roadmap to virtual program implementation and our evidence-based journey to success:
- Innovate a new staffing model to address the nursing shortage, provide safe distribution of workload, and reduce salary expenses
- Improve patient outcome metrics
- Improve early intervention for patient deterioration through utilization of the electronic medical record (EMR) applications and artificial intelligence (AI) alerts to enhance monitoring and improve timely response times
- Improve employee engagement
In addition, outcome metric selection included the following core and fundamental categories essential to program success:
- Quality
- Finances
- Recruitment and Retention
- Epic (Epic Systems Corporation, 2023) EMR Documentation
Virtual Nurse Program Design
The Virtual Nurse Program adopted a nursing care model different from many traditional models that healthcare institutions have had in place for the last several decades. The model moved away from individual nursing (i.e., a modified primary nursing model), which relies on one professional nurse to address all patient care tasks. It instead is based on a team model in which all disciplines can work at the top scope of licensure, consequently balancing the workload more effectively across the patient care team throughout the hospital stay (Denney & Evans, 2017; Russell, 2023).
The Virtual Nurse is employed from a remote location (e.g., home, or a bunker housing a group of VNs) in real time, working in tandem with teams of RNs, licensed practical nurses (LPNs), and patient care technicians (PCTs), to establish a collaborative professional approach for each patient assignment. A virtual nurse program accomplishes this through selected responsibilities and workflows that emphasize the importance of the bedside RN/LPN role. In contrast with consultative virtual models seen with eICU platforms (Udeh et al., 2018), the Virtual Nurse Program operates strictly within a team-based framework, where each team member shares responsibilities and supports one another to accomplish equivalent goals within the patient plan of care.
Such a framework allows ongoing collaboration between virtual and bedside nursing teams and other providers, such as pharmacists, case managers, and other ancillary or support services involved in the patient’s care. The end result is a synchronized plan of care and actions to attain established patient goals. Figures 1 and 2 illustrate the Virtual Nurse Program design and the divisions of roles and responsibilities of the care team.
Figure 1. Virtual Nurse Program Design
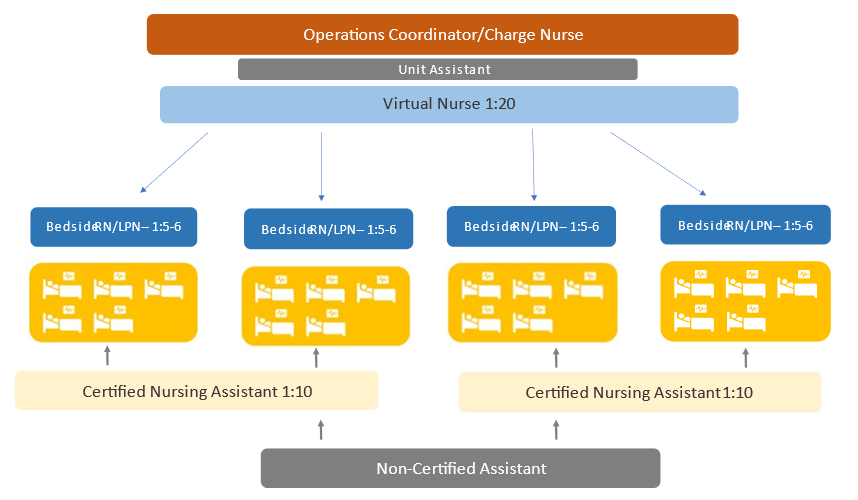
Figure 2. Roles and Responsibilities of the Patient Care Team
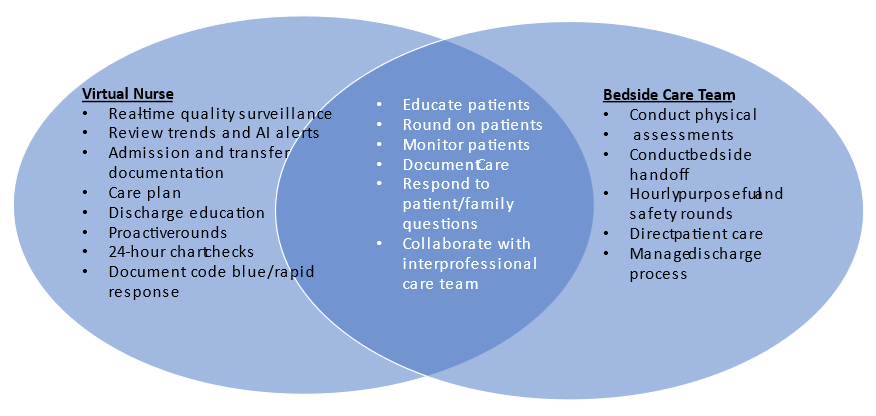
As a member of the care team within this model, the Virtual Nurse plays a significant role in the completion of documentation. Continued surveillance of documentation compliance, especially as it pertains to clinician follow-up of critical interventions that determine essential steps in quality of care or early intervention, is a pivotal benefit of the Virtual Nurse EMR workflow. ‘Behind-the-scenes’ evaluations and ongoing monitoring of important patient clinical information guarantee a secure pathway for optimal and timely intervention and positive results.
The Value of the Virtual Nurse Investment
The value of the Virtual Nurse Program has expanded across several areas that have an important impact on organizational quality and patient safety outcomes; the well-being of the workforce; and cost avoidance measures and nursing model optimization. These positive impacts exemplify the benefits of an HRO mindset.
Patient Safety
The most important benefit of this program has been the impact on patient safety and the early detection of deterioration of the patient’s health condition. The Virtual Nurse activates proactive rounds or rapid response interventions based on ongoing review of patient Modified Early Warning Scores (MEWS), clinical review of vital signs, laboratory values, clinician notes, and virtual assessment of the patient to validate decompensation triggers (Institute for Healthcare Improvement, 2023). AI alerts that the Virtual Nurse receives through the EMR platform also trigger mechanisms for immediate clinical evaluation and response. These methods allow fast notification of the clinicians needed to offer the best options and disposition for every patient in a timely manner. In addition, utilizing these processes decreased hospital Code Blue events outside of the intensive care unit (ICU), avoided ICU transfers, maintained the sepsis risk-adjusted mortality index (RAMI), and lowered expected overall mortality rates.
Another valuable benefit of the Virtual Nurse Program as it relates to patient safety centers around 30-day readmissions. Virtual Nurses play an essential role in the discharge process; hence, there is value in providing this resource to ensure a seamless post-hospital transition. Several factors contribute and affect hospital readmissions (Herzig et al., 2016). However, the valuable time spent 1:1 with every patient at the time of discharge allows for specific questions, instructions, or family conversations that can prevent typical reasons for readmissions. The influence of the Virtual Nurse on the discharge process and patient education has successfully reduced hospital readmissions, generating substantial finance capture related to direct cost avoidance.
Standardized Quality
Besides the important contributions of the Virtual Nurse to patient safety and clinical outcomes, the program’s design drives and facilitates inpatient throughput (while not compromising care quality) within the admission and discharge process. Virtual Nurses perform the vast majority of admission and discharge documentation as they virtually conduct the non-bedside parts of these processes. The Virtual Nurse works alongside the bedside care team to complete details necessary to expedite accurate follow-up as patients transition through distinct phases of care. Through this, the Virtual Nurse promotes care standardization as the team member responsible for admissions, discharges, and documentation.
By having the Virtual Nurse lead Admission/Discharge/Transfer (ADT) functions in the organization, we have gained insight into processes that affect overall patient length of stay or appropriate post-acute placement, such as medication reconciliation, progressive mobility, and device utilization. This is critical in fast-paced units with high patient volume and turnover. Multiple social challenges and family dynamics (e.g., post-acute placement options, differences in family member opinion related to plan of care, variations in disease process education, etc.) can create throughput gridlocks and disposition risks following the hospital stay. Virtual Nurses achieve accuracy and efficiency through multidisciplinary collaboration for every patient before discharge.
The Virtual Nurse Program also achieves clinical standardization by decreasing variation in required procedural timeouts during bedside procedures and device utilization surveillance maintenance. Virtual Nurses oversee a variety of bedside procedures, such as central line placement, ensuring process and documentation accuracy. One role responsibility includes device observation and scrutiny with bundle compliance, consequently driving device utilization precision and reduction in hospital-acquired infections. Another benefit is the assistance provided to bedside nurses, saving their valuable time to focus on other hands-on bedside tasks. This time savings reduces clinical burnout due to managing multiple responsibilities that, by default, often become nurse-led. The Virtual Nurse Program value not only supports an innovative approach to patient care management but also offers a fresh look to professional nursing in medical-surgical units, where nurses can have overwhelming workloads and frequently are the sole provider of care rendered.
Lessons Learned
As with any major project implementation, change brings challenges and unexpected barriers throughout every phase. Our most valuable lessons were related to the time and resources needed to manage teambuilding and growing the relationships that the team required to succeed. Creating connections and bonds that result in trustworthy partnerships requires stakeholder buy-in. For this to occur, all parties had to commit to adopting creative ways for collaboration through shared patient responsibility. Overcoming the old way of doing things to welcome something different was the most challenging part of this project.
Nurses were accustomed to performing individually; therefore, the idea of sharing a patient assignment with someone not physically present in the same space was a difficult change. Multiple teambuilding sessions and communication resources were necessary as the project moved through each phase. Defining the new roles and providing clarity of role responsibility was critical to identify opportunities, find neutral ground where roles could merge, and for the nurses to see the value in others’ contributions. These challenges can occur within any team but require extra attention in the virtual environment because of the lack of in-person interaction between team members (Russell, 2023).
In the beginning, recruitment of Virtual Nurses was difficult as the role was very new in the profession of nursing, and not yet attractive to potential candidates. There was contract labor expense associated as the project began, to support both bedside and virtual nursing positions needed. Despite challenges, all lessons learned helped us to develop confidence, and solidify the leader, and nurse comfort levels in the program value. Benefits such as those described above were evident from the very beginning and have continued to improve. At this time, our nursing teams cannot envision rendering high-quality care or managing effective operations without Virtual Nurses as contributor to the care team.
“WINS” for our Most Valuable Asset: Our People
The benefits of the Virtual Nurse Program would not justify its value if it did not positively contribute to the workplace environment and engagement of the team. Despite the clinical outcomes and fiscal advantages, the most significant merit of the program is the support and expertise provided to our nursing teams. Whether it is an inexperienced nurse receiving help with task management or expert advice with clinical decision-making, a seasoned travel nurse accepting collaboration to expedite the rapid response process, or a float pool employee getting assistance with multiple discharges and admissions, Virtual Nurses are fundamental to each scenario. They establish clinical presence, expertise, and exercise the core values that shape nursing. This patient-focused care model relies on the value of our people through teamwork, communication, and professional excellence.
A Virtual Nurse provides 24-hour support and visualization of assigned patients, providing real time human connection through frequent interactions that allow the entire care team to gain a full picture of multiple aspects of the patient’s care. In so doing, regular communication among the care team becomes engrained in daily practice and creates a sense of dependency across team members. Particularly for nursing staff, this type of team model secures a “second set of eyes” that at times is pivotal to determining the clinical interventions needed to place the patient in the best level of care.
Sharing responsibilities of virtual and bedside nurses within the patient’s plan of care can develop professional, emotional, and personal supports that enable confidence in peer skillsets. This model provides a different level of professional practice that enhances nurses’ trust in their peers and facilitates understanding of the value of all contributors in daily work practice. The end goal of this care model is stable or increased nurse engagement, which consequently strengthens the work environment, and teamwork, yielding lower turnover.
The hospital initiated this care model in 2018, just prior to the COVID-19 pandemic, so although consistent downward trends in turnover percentage are not evident year over year, the actual number of bedside nurses leaving the organization has declined. The fact that employee engagement and bedside RN turnover remained consistent or improved during the pandemic years is a testament to the success of this virtual care model and our team.
Clinical Collaboration
Since its inception, several other disciplines have taken advantage of the virtual platform to expand patient care opportunities. The Virtual Nurse Program has opened the door for virtual hospital medicine physicians who offer support to onsite medical teams through review of patient conditions, order entry, non-emergent patient follow-up, and other key functions that promote provider collaboration. Within the same platform, remote Advance Practice Providers (APP) assist with night shift rounds, respond to calls from nurses requesting specific information or patient requests, and finalize discharges in situations with post placement challenges or special family concerns.
Some specialty services have also used the virtual care platform to expand availability after hours and on weekends when there may not be onsite coverage. Through a compatible video application, physicians can evaluate a patient remotely when a clinical concern presents. They are also able to answer questions or address concerns from anywhere in the hospital by simply logging into a hospital-based PC or laptop. This particular feature was extremely valuable during the COVID-19 pandemic when clinical teams struggled with personal protective equipment supplies and other resource challenges.
Other disciplines, such as pharmacy and case management, have joined the virtual platform by adopting workflows to address regular duties virtually, thereby expanding capacity and expediting processes within their roles. For example, the pharmacy has used the Virtual Nurse technology to perform medication reconciliation remotely, and in so doing, reach a larger number of patients to provide 1:1 checks-and-balances, education, and quality assessments. Case managers are exploring ways to use this platform to discuss patient placement options with family members, share insurance coverage information, and optimize solutions based on a patient’s best interests and plan of care. This could expedite the discharge process and avoid rework, reduce workflow delays, and improve all-around team collaboration to promote throughput efficiency.
Next Steps
The Virtual Nurse Program is just starting to realize the many options available to address significant opportunities in hospital operations, care model standardization, and in bridging gaps to the future in nursing and in healthcare overall. This innovative technological approach facilitates ‘top of license’ practice for participating clinicians, extends access to provider collaboration, and most importantly, enhances the work experience of the nursing workforce to promote retention and teamwork, thus promoting highly engaged teams. As we have experienced in the last five years, this program has changed the form, structure, nursing workflows, and general scope, making it a critical part of care delivery in our hospital.
Nursing and information technology leaders, along with executive and multidisciplinary partners, are continuously working to optimize the current care model and ensure that it is meeting the needs of patients and staff. They evaluate and integrate new EMR tools, such as pathways and workload intensity measures, to boost Virtual Nurse efficiency and effectiveness. As we continue our journey, program evolution is also under discussion, including options for spreading and scaling, and future possibilities such as Virtual Nurse contributions to “hospital at home” programs, especially those pertaining to patient education and/or communication.
Recommendations for Practice
Based on our journey with the Virtual Nurse Program, recommendations center around the general goals and purpose for this organizational change. Because the virtual platform offers several options for implementation, it is important to outline specific reasons to initiate this model within current nursing practice. For example, it is essential to identify the best approach to formulate an appropriate business case, and to carefully outline both clinical and financial outcomes expected from care model implementation.
This type of care model is a significant investment for any institution; hence, it is important to set both short- and long-term goals for return on investment (ROI), founded on realistic measures of success. For instance, a focus on nurse-to-patient ratio expansion as an ROI may not generate expected quick financial wins, as the introduction of a new virtual model may not be the single solution to expand ratios without a detailed assessment of both existing and required bedside support. Instead of focusing on fast labor reduction as a main performance indicator, our recommendation is to address the full scope of the organizational need and set ROI goals that include both hard dollar and soft cost-saving projections for optimal (and realistic) program benefit allocation.
Another suggestion to consider is the type of staffing model to implement, and how this initiative will balance workforce resources within the organization. In particular, is it worth considering the impact of having a team who works solely virtually as a separate entity from bedside staff? In addition to considerations about how to facilitate collaboration and trust between virtual and bedside staff (Hoonakker et al., 2017; Russell, 2023), resource allocation or distribution will also vary depending on the choice of virtual team selected. Purely virtual (i.e., remote) teams will require additional nursing resources, as they will remain completely independent from the bedside through onboarding of separate virtual nurse staff.
Models that set parameters around shifts worked at the bedside along with shifts worked in the virtual setting can adopt shared resources. Consequently, nurses could work in both the bedside and virtual settings. It is in the best interest of the organization to evaluate the pros and cons of each type of staffing model, as resource optimization becomes pivotal for program success and sustainability. Regardless of the model selected, the organization must regularly evaluate and design leadership structure and program oversight, to ensure that foundations of team-centered core values are consistently and sufficiently hardwired for program success.
Lastly, detailed consideration of defined roles and responsibilities must be performed initially (Russell, 2023) to avoid the virtual nurse role from becoming the ‘catch all’ for multiple duties that may be passed along. The organization must clearly identify virtual scope of practice, so that Virtual Nurses provide true and reliable support for bedside staff and can accomplish the tasks intended to yield expected results. Narrowing the scope initially to demonstrate program value may offer a quicker rollout with limited tasks and logistical span on which to pilot workflows and potential barriers that may interfere with planned implementation phases. Greater transparency around roles, responsibilities, and expectations of performance will result in greater engagement across teams and connection to project purpose.
Recommendations for Research
Implementation of virtual nursing care models outside of the ICU is still relatively new. There are many opportunities to conduct empirical research to evaluate program optimization and examine outcomes associated with this innovative model. There is a need for research to investigate how virtual roles impact the overall nursing workforce. One specific area of interest is nurse satisfaction and retention. It has been suggested that a hybrid virtual model can positively impact retention by allowing nurses to remain in direct patient care while decreasing physical demands of the bedside nurse (Cloyd & Thompson, 2020). Long-term studies exploring nursing career trajectories and the contribution of virtual roles would provide direction for new role creation.
Another area for research is the patient experience of virtual care. Previous research has shown that patients have reported high levels of satisfaction with telemedicine interventions (Eze et al., 2020) and that patient experiences with virtual care visits were not substantially different than with in-person visits, particularly during the COVID-19 pandemic (Bilimoria et al., 2021). However, there is still much to explore with patient experiences and virtual inpatient care. At one setting that had implemented a hybrid virtual inpatient nursing model, the majority of patients preferred rooms with virtual nurses, but there were still challenges to overcome in patient understanding of the technology and role of the Virtual Nurse (Schuelke et al., 2019).
Evaluating the impact of programs on those disciplines directly involved with care of patients, while driving quality and operational results, can provide evidence of the value of virtual care models to overall organizational success. As different disciplines pilot virtual platforms, there will be opportunities to explore additional workflow or process efficiencies and teamwork collaboration in the virtual environment.
Finally, our experience with the Virtual Nurse Program is exclusive to a community hospital and the dynamic within that setting. Future research needs include examining implementation and outcomes of this virtual care model in additional settings, such different geographical areas, patient populations, and organizational and health system components.
Conclusion
The Virtual Nurse Program is multifaceted and offers a variety of workflows and prioritization options to target a variety of inefficiencies that an individual organization might experience. Such a care model can adapt to the differing needs of hospitals and can use the same resources to create additional options to enhance clinical practice at multiple levels. The Virtual Nurse model allows hospitals to utilize resources in the best possible manner, to augment bed capacity, enhance quality of care, and strengthen their workforce. Hence, in practice, the value of virtual care models can reach as far as the implementation goal extends.
Authors
Ruth Sagastume, MSN, RN, CPHQ
Ruth Sagastume is the Chief Nursing Officer at Ochsner Medical Center – Kenner River Region. She began her career at Ochsner Health 27 years ago and has held leadership roles in nursing operations and performance improvement. Ruth received a nursing diploma from Charity School of Nursing, and BSN and MSN degrees from the University of Phoenix. She is a Certified Professional Healthcare Quality.
Jessica Peterson, PhD, RN
Jessica Peterson is the Senior Nurse Researcher at Ochsner Health. Prior to joining Ochsner she worked in academia teaching research methods at the graduate level. Jessica received a PhD from the University of Toronto.
